There is an old saying that practice makes perfect. It is the main reason that a basketball player will shoot hours of jump shots or a musician will play a new musical piece over and over. Their goal is to take their craft and make it as flawless as possible. It is also the same reason that Wellington Regional Medical Center (WRMC) practices and tests possible disaster situations.
Practice drills can cover any situation from hurricanes or tornados to a mass-casualty situation that result in a large number of patients arriving at the hospital in a short period of time. The ultimate goal is to make sure that the hospital is ready for a surge of patients. WRMC had a drill on Thursday, March 19, and it was the third in less than two weeks regarding COVID-19, otherwise known as the coronavirus. Specifically, the most recent drill focused on the best and safest way to triage and transfer an influx of patients into the emergency department for treatment.
“It is vital for healthcare organizations to think through scenarios that might happen and then pressure test them to look for points where we might fail,” WRMC CEO Pam Tahan said. “Once we find those different areas we need to address, we can make adjustments. The drills allow us to improve our processes to make patients, guests and staff safer when they come to Wellington Regional.”
As part of the COVID-19 preparations, WRMC began screening all patients and visitors for symptoms of COVID-19. In addition, the hospital started asking about visitors’ possible exposure to the virus, including international travel in the past 14 days, exposure to a known patient with coronavirus in the past 14 days, and any COVID-19 symptoms such as cough, fever or shortness of breath.
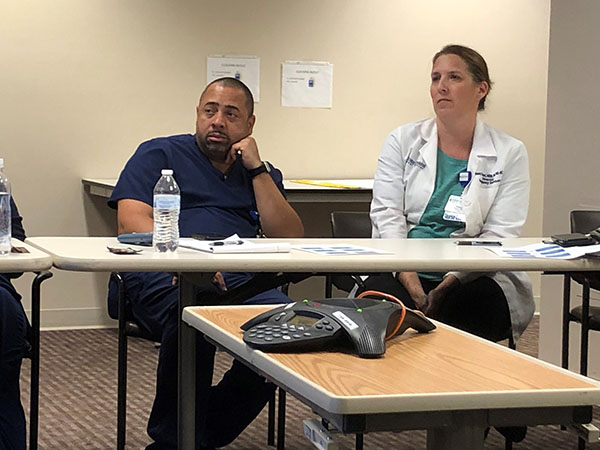
WRMC Director of Risk Management Brenda Atkins guided the group of hospital and nursing leaders through a COVID-19 situation. Participating in the drill are physicians as well as representatives from the emergency department, infection control, respiratory, admissions, radiology, pharmacy and administration.
Atkins provided various scenarios to the group to resolve. Once a problem is solved, it leads to the question, “OK, then what happens?” That way, any solution can be looked at from multiple angles to make sure the resolution is in the best interest of caring for the patient, as well as protecting visitors and hospital staff. The topic of the most recent COVID-19 drill: five patients arrive at the emergency department with known exposure to COVID-19 and are experiencing symptoms.
Initial conversations center on the best way to move the five patients to rooms inside the department for examination, while diminishing the possible exposure to staff and other visitors inside the hospital. Discussions are detailed and even include examining the best and most efficient rooms to use for the patients’ care inside the emergency department. Once the theoretical patients were transferred for treatment, the conversation shifted to the appropriate use of personal protective equipment (PPE), as well as the best way to put PPE on and how to remove it to limit exposure or cross-contamination in the emergency department.
“Once we have found the best way to transfer the patients to the room, we are triaging them to better determine their symptoms and condition,” said nurse Stacy Morast, director of the emergency department. “The nurses and doctors will assess and treat the patients once they have safely been transferred into the rooms.”
The drill continued with the disclosure that one of the patients is a person of interest for COVID-19 per the Centers for Disease Control and the Florida Department of Health guidelines. The room then began to discuss the phone tree of people that need to be notified that a suspected COVID-19 patient is in the hospital, including calls to the Florida Department of Health. “We have put together a crisis plan that lists all the phone numbers that need to be notified if we have a suspected patient,” Morast said.
The confirmation by the department of health is vital to allow testing of patients. “OK, the Florida Department of Health has indicated that the patient meets the qualifications to be tested,” Atkins said. “What are the specimens that need to be collected and where do we send the samples?”
The drill concluded with the group walking through the collection techniques and steps required to ship the samples for testing. In this situation, the patients were not critical enough to require admission to the hospital, so the group discussed the discharge process and the safest route to exit the patient from the emergency department and limit exposure to others.
There was also discussion about misinformation that exists, including patients being told physician offices can’t do tests or that only emergency departments can perform the COVID-19 test. Further public confusions include that only emergency rooms can clear a person to return to work after being sick or travelling internationally.
The current recommendations by the CDC and the Florida Department of Health are for patients who are not critically ill to remain at home and self-isolate for 14 days. Individuals should be sure to hydrate, take over-the-counter medications for fever, rest and eat well during the recovery period. There is currently no “cure” for COVID-19, except time, and patients are currently treated by addressing the symptoms of the illness. Only patients who are critically ill will be admitted to the hospital for symptom treatment.
Wellington Regional is providing updated COVID-19 information at www.wellingtonfl.gov/coronavirus.
COVID-19 Information From WRMC
• The coronavirus is in the same family with the virus that causes the common cold. Most everyone has already been exposed to a type of the coronavirus in their lifetime.
• For the vast majority of the people who are positive for the virus, they will only have the symptoms of a common cold. The people at the highest risk for complications are people over age 60 and people who have other medical conditions, such as diabetes, a heart condition or respiratory conditions.
• Practice social distancing, avoid crowds, avoid shaking hands, and avoid touching your face, eyes, mouth and nose.
• Wash your hands frequently with soap and water for at least 20 seconds. If soap and water is not available, a hand sanitizer with at least 60 percent alcohol can be used as a substitute.
• Only people who meet the CDC guidelines for testing will be tested for the virus. This can change as the CDC changes its guidelines.
• If you are not experiencing symptoms of COVID-19, a test will not be helpful. COVID-19 can only be confirmed if a person is having symptoms. A test to “rule out” the virus is not helpful if a person is not having symptoms.
• The symptoms of the virus may include fever, shortness of breath and cough.
• The incubation period for COVID-19 is between two and 14 days.
• There is no treatment or cure for the virus; only the symptoms are treated.
• If you need to go to your doctor, call ahead and let them know you are coming, so they can be prepared for your arrival.
• If you are in medical distress, call 911.